Introduction
Self-management is in the crucial role in controlling chronic illnesses and maintaining quality of life for patients living with chronic conditions (Eller et al., 2018; Jaarsma et al., 2017). Care of these conditions mainly happens, not in hospitals nor by professionals, but at home by patients and their significant others during every-day living (Campbell et al., 2018). Self-management can be demanding for patient and their close ones in different ways. It needs sufficient skills and knowledge, but also motivation and emotional endurance. (Cramm & Nieboer, 2013.) More and more attention is paid in healthcare on enabling and supporting the self-management skills of patients with chronic illnesses and how the self-management education can be delivered (Heggdal et al., 2021). In addition to hospital-based programs, it can be organized utilizing different approached such as community programs (Mulligan et al., 2019). It is noteworthy to recognize the role of the digital self-management support through online interventions (Vassilev et al., 2015). However, patients with chronic conditions should also be involved in the developing process of the self-management interventions which are aiming to enhance self-management abilities (Donald et al., 2018).
This literature review provides information on the various benefits patients and their family received from different self-management support services and interventions by health care professionals. The research question was: How self-management support organized by health care has benefited patients with chronic diseases and their family members?
Methodology
This literature review by Tampere University of Applied Sciences (TAMK) was a continuation of the work started by the Hanoi Medical College (HMC) on the same topic. The complementary data search was conducted using the CINAHL database limiting to peer reviewed articles published within 2020-21. The articles found by the HMC were reviewed by TAMK and the results answering the research question were added as manual search results to the data. In conclusion of the searches, 16 articles, from Canada, Australia, Germany, Bangladesh, Nigeria, UK, USA, Switzerland, Norway, and China were included in the analysis (Figure 1). Eight of the research were quantitative, four qualitative and four conducted using mixed method. The data was analyzed using inductive qualitative content analysis.
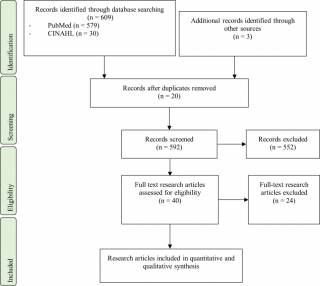
Figure 1. A PRISMA flow chart
Results
Patients with chronic diseases and their family members benefited from self-management support organized by health care in physical, emotional, cognitive, and social levels resulting to comprehensive self-management governance. They gained strengthened ownership of self-management, more advanced health literacy competencies and started implementing healthier lifestyle which improved state of well-being and, also, resulted active reciprocal interactions in their relationships (Figure 2).
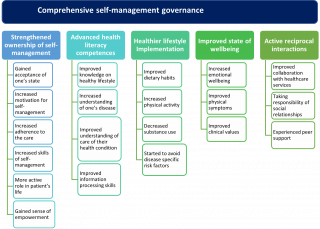
Figure 2. Main and sub-categories
Strengthened ownership of self-management
Self-management support organized by health care benefited patients with chronic diseases and their family members by strengthening ownership of self-management. This includes gained acceptance of one’s state (7, 13), increased motivation for self-management (1, 7, 11, 13), increased adherence to the care (2, 5, 10, 11, 12, 13, 15, 16), increased skills of self-management (2, 5, 6, 7, 9, 13, 14, 16), more active role in patient’s life (7, 11, 12, 13, 16) and gained sense of empowerment (2, 5, 6, 7, 11, 13, 16).
Through interventions and programs provided by health care, patients gained acceptance of one’s state. They had more positive attitude towards their disease (13) and by the end of the programs they could live with their state (7, 13). The acceptance of the disease facilitated the experience of returning to normal life (7), determination for an active life increased initially and patients participated in daily life more than before despite illness-related challenges (13). They learned the feelings of being angry is part of the approval process (13).
Self-management support organized by health care increased patients’ motivation for self-management which was reflected in their increased motivation to set goals (13). Patients also became motivated to possess their health (11), started to do things they used to be unwilling to do (7), and their motivation to engage to physical activities increased (11). Moreover, one intervention helped patients to start correcting their life situation from the onset and progression of the disease (7). Other interventions increased patients’ willingness to dedicate time for their plan to achieve stability and maintenance of the long-term management of chronic illness (16) and patients’ intent to self-manage his/her follow-up care (1).
Increased adherence to the care appeared in patients’ accountability (16) and commitment to their treatment (2, 5, 10). It was made possible e.g., by information of how to engage in their care (12). Patients also engaged in learning the techniques to manage their disease (16). Through interventions and other support organized by health care patients’ adherence in taking their medicines strengthened (5, 11), they used their medications more effectively (5) and followed their medication administration schedule (13). Patients also engaged in the exercises (16) and were more likely to walk at least five times a week (15).
Patients’ increased skills of self-management were evident after interventions implemented by health care (2, 5, 6, 7, 9, 13, 14, 16). Patients were able to assess their skills in self-management activities (13), assess and identify their needs for follow-up (7) and health (7) and manage their disease (8, 13, 14). Developing own self-management strategies was also easier for them (13). Moreover, informative support helped patients to be more effective in their technology use (16).
Patients and their family members took more active role in patient’s life. After getting self-care support from health care, patients realized that they should be actively involved in managing and improving their own health (11) and they became more active in their lives (7). Participants took more initiative (16), started to prepare for their visits with healthcare providers (13), and they began to seek more information about the disease and search information from several sources (11). They also realized that they needed to be more assertive to get understandable information (12). After getting health care provided self-care support patients started to prioritize things and goal setting was easier for them (13). They also learned how to engage in health-related activities, and they were able to perform free time activities (11). Moreover, family members supervised training of their next of kin (11). The informative support from health care worker helped even in trouble-shooting technology issues (16).
When participating in self-care support activities patients gained sense of empowerment. Patients’ confidence of self-care increased (2, 5, 6, 13, 16). Support provided subjects reassurance (16) and their confidence in coping with their symptoms and self-management skills strengthened (11). They felt more powerful (11), their self-efficacy improved (13) and they were able to discover something new about themselves (7). For some patients, knowledge of their own abilities and what they want became clearer (7). They wanted to advocate for themselves (13) and the received support enabled patients to be taken as experts in their own medical experiences (7). They were more aware of their self-care behavior (2) and their own responsibility in the management of their disease (11). The patients were able to plan their health promotion processes (7), they were empowered in decision making in their health issues (6) and they started to develop new self-management strategies (13). Some patients resumed self-care (13).
Advanced health literacy competences
Advanced health literacy competences included improved knowledge on healthy lifestyle (4, 6, 11, 13), increased understanding of one’s disease improved (1, 5, 7, 9, 10, 11, 12, 13), understanding of care of their health condition (5, 7, 11, 16) and improved information processing skills (11, 13).
Improved knowledge on healthy lifestyle in research papers showed in patients getting useful information for everyday life (13) and becoming aware of physical activity, unhealthy drinking, and unhealthy eating habits. (11); e.g., the level of knowledge of salt and diet modification increased (4). The programs helped the patients to learn knowledge of prevention (11) and the knowledge a person has in managing their own health and care improved significantly (6).
By help of health care, increased understanding of one’s disease overall was reached by patients (1, 5, 7, 9, 10, 11) and family members (11). They became aware of the severity (11) and the prognosis of the disease (11) as well as about how the disease progresses (11). They learned what contributes the development of the disease (11) and the uncertainties of the disease for patients (12). Patients’ knowledge of their condition increased (5, 12, 13) and some patients were able to identify their exceeded comfort zones within their own physical limits (7).
Interventions improved patients’ and their family members’ understanding of care of their health condition. Their understanding what is smart for oneself increased (7) and the patients became aware of the importance of avoiding risk factors for their disease (11). Patients increased their knowledge in managing their own health and care (5, 11) and the same was reached also by their family members (11). Through the support provided by health care understanding of rehabilitation increased (11) and the reasons for daily tasks to control the disease became clearer (11, 16); e.g., understanding of respiratory training and respiratory training techniques (11). Knowledge of patient’s medication increased (5, 11) as well as management of their medication (11). Patients’ knowledge of services that can help managing self-care increased as well (5).
Improved information processing skills were evident within patients when they became more aware of the importance of knowledge of the disease (11). They also got trustworthy information (13). The interventions taught them to search for information to understand their illness (11) and based on information they didn’t fear for the drug dependence anymore (11).
Implementing healthier lifestyle
During and after various interventions, patients started implementing healthier lifestyle. They improved dietary habits (4,11,13,15), increased physical activity (3,7,11,15), decreased substance use (11,15) and started to avoid disease specific risk factors (11).
Improved dietary habits meant that the patients ate healthier food (13) and avoided unhealthy food (11). Also, the practice of diet and salt restriction improved after intervention (4) and patients’ fruit intake practice increased significantly (15).
Increased physical activity showed in significant increase of participants’ mean number of days of exercise per week and mean hours of exercise per day increased a little (15). Supported by health care, the patients began to participate in more activities to control their symptoms (11) for example starting a swimming course (7). In one intervention, participants improved physical activity with help of app reminder function (3).
Health care interventions for self-management support decreased substance use, including participants being more likely to quit using smokeless tobacco and betel nut (15) and avoiding passive and active smoking (11). Participants’ use of smokeless tobacco, chewing tobacco (e.g., Jorda, Gul), and betel nut decreased three times during intervention (15) and use of smoke tobacco or cigarettes decreased a bit during intervention (15).
With self-management support by health care, the patients started to avoid disease specific risk factors. The participants began to avoid risk factors (11), like high cooking fumes (11) and unhealthy behaviors (11). The participants also began to wear a mask (11) and to keep themselves warm outside. (11)
Improved state of well-being
Self-management support benefited patients with improved state of wellbeing, which included Improved physical symptoms, Improved clinical values and Increased emotional wellbeing.
Improved physical symptoms showed in reported improved physical health component HRQoL (Health Related Quality of Life) (9). The participants stayed healthy (11) and had fewer health complaints. (13) Self-management support led to improvements in breathing (16), also from perception of the participants (16). Patients learned how to breath comfortably (11) and their breathing performance improved (11).
Improved clinical values included patients’ decreased systolic blood pressure, weight, BMI and HDL cholesterol level, (5) improvement of more than half of the measured scores after intervention (5) and improvement of participants’ blood glucose levels significantly (15), including significantly lower mean HbA1c level (8). In one intervention, glycemic control improved (14), for example each blood glucose value sent via SMS reduced HbA1c levels in long run (14).
Increased emotional wellbeing meant that patients got a range of emotional and psychological benefits (16), reported improved mental health component in Health Related Quality of Life (9), became more hopeful (7) (13), felt accepted (13), encouraged (16), better emotionally (11), and more optimistic (11).
Trough the self-management support by the health care, the patients were more capable to handle their depressed feeling (13) and were not overwhelmed by difficult emotions anymore (13). The patient received confirmation that his/her thoughts and feelings were valued inputs to her/his own recovery (7) and patients who have had the disease for a long time realized that they had an on-going grieving process (7) and were allowed to be sad (7) and so achieved some empathy for themselves (7). Patients felt that they were understood by the health care providers (16).
Active reciprocal interactions
Through self-management support by the health care, patients were able to achieve active reciprocal interactions in forms of improved collaboration with healthcare services, taking responsibility of social relationships and experienced peer support
Improved collaboration with healthcare services meant that access to health care professionals became easier (11) and the participants had more opportunities to get help from health care professionals (11). The participants became aware of the mutual responsibility of health care worker and themselves (11) and established a more confidential relationship with health care providers. (13) Also, participants’ usage of National Health Service’s cost significantly less after one intervention (5).
Grown responsibility of social relationships got established by understanding the meaning of patient’s own input, which made patients less angry and more co-operative with their family (7). Also, Family members learned how to support the patient (11). Self-management support helped to strengthen the social support network by developing new effectively communicated views (7). Grown responsibility in social relationships was also manifested by participants coaching other patients (11) and sharing their knowledge (11).
Experienced peer support provided an opportunity to compare their own experiences (7), receiving compassion from peers (7) and feeling of not being isolated in the peer group (13). Peer leaders unified participants (13) and the group process facilitated recovery (7).
CONCLUSIONS
The results show how health care has essential role in self-management support, and how it is effective and necessary for successful self-management of chronic diseases.
Patients and their families had wide range of benefits, which underlines how the self-management support should be extensive. Patients and family members strengthened their ownership of self-management and advanced their health literacy competencies. Through self-management support, patients and family members implemented the gained competences of healthier lifestyle, improving their well-being and active reciprocal interactions in their relationships.
Family members’ perspective was hardly represented in the data, as their perspective was very little researched. However, when included in the research, family members participation in self-management was important.
Educating health care students to offer extensive self-management support, including family members, is essential to gain competences to offer this support. Variety of self-management support skills are needed, and this variety should be reflected in the educational DigiCare model.
References
Campbell, F., Lawton, J., Rankin, D., Clowes, M., Coates, E., Heller, S., De Zoysa, N., Elliott, J., & Breckenridge, J. P. (2018). Follow-Up Support for Effective type 1 Diabetes self-management (The fused model): A systematic review and meta-ethnography of the barriers, facilitators and recommendations for sustaining self-management skills after attending a structured education programme. BMC Health Services Research, 18(1), 898. https://doi.org/10.1186/s12913-018-3655-z
Cramm, J. M. & Nieboer. (2013). The relationship between self-management abilities, quality of chronic care delivery, and wellbeing among patients with chronic obstructive pulmonary disease in The Netherlands. International Journal of Chronic Obstructive Pulmonary Disease, 209. https://doi.org/10.2147/COPD.S42667
Donald, M., Kahlon, B. K., Beanlands, H., Straus, S., Ronksley, P., Herrington, G., Tong, A., Grill, A., Waldvogel, B., Large, C. A., Large, C. L., Harwood, L., Novak, M., James, M. T., Elliott, M., Fernandez, N., Brimble, S., Samuel, S., & Hemmelgarn, B. R. (2018). Self-management interventions for adults with chronic kidney disease: a scoping review. BMJ Open, 8(3), e019814–e019814. https://doi.org/10.1136/bmjopen-2017-019814
Eller, L. S., Lev, E. L., Yuan, C., & Watkins, A. V. (2018). Describing Self-Care Self-Efficacy: Definition, Measurement, Outcomes, and Implications: Describing Self-Care Self-Efficacy. International Journal of Nursing Knowledge, 29(1), 38–48. https://doi.org/10.1111/2047-3095.12143
Heggdal, K., Mendelsohn, J. B., Stepanian, N., Oftedal, B. F., & Larsen, M. H. (2021). Health‐care professionals’ assessment of a person‐centred intervention to empower self‐management and health across chronic illness: Qualitative findings from a process evaluation study. Health Expectations, 24(4), 1367–1377. https://doi.org/10.1111/hex.13271
Jaarsma, T., Cameron, J., Riegel, B., & Stromberg, A. (2017). Factors related to self-care in heart failure patients according to the middle-range theory of self-care of chronic illness: A literature update. Current Heart Failure Reports, 14(2), 71–77. https://doi.org/10.1007/s11897-017-0324-1
Mulligan, H., Wilkinson, A., Chen, D., Nijhof, C., Kwan, N., Lindup, A., & Dalton, S. (2019). Components of community rehabilitation programme for adults with chronic conditions: A systematic review. International Journal of Nursing Studies, 97, 114–129. https://doi.org/10.1016/j.ijnurstu.2019.05.013
Vassilev, I., Rowsell, A., Pope, C., Kennedy, A., O’Cathain, A., Salisbury, C., & Rogers, A. (2015). Assessing the implementability of telehealth interventions for self-management support: A realist review. Implementation Science : IS, 10(1), 59–59. https://doi.org/10.1186/s13012-015-0238-9
Literature review:
- Mutsaers, B., MacDonald-Liska, C., Larocque, G., Morash, R., Stenason, L., Harris, C., & Lebel, S. (2021). An evaluation of a cancer survivorship education class for follow-up care. Canadian Oncology Nursing Journal, 31(1), 51–56. https://doi.org/10.5737/236880763115156
- Chen, S. H., Boyd, J., Randall, S., & Maiorana, A. (2021). Association between community-based nurse practitioner support, self-care behaviour and quality of life in patients with chronic heart failure. Australian Journal of Advanced Nursing, 38(3), 25–32. https://doi.org/10.37464/2020.383.147
- Steinert, A., Eicher, C., Haesner, M., & Steinhagen-Thiessen, E. (2020). Effects of a long-term smartphone-based self-monitoring intervention in patients with lipid metabolism disorders. Assistive Technology, 32(2), 109–116. https://doi.org/10.1080/10400435.2018.1493710
- Ajiboye, R. O., Okafor, N. A., Olajide, T. E., & Tosin, E. O. (2021). Effect of Nursing Intervention on Knowledge and Practice of Salt and Diet Modification among Hypertensive Patients in a General Hospital South-West Nigeria. International Journal of Caring Sciences, 14(1), 392–400. Retrieved from https://libproxy.tuni.fi/login?qurl=https%3A%2F%2Fwww.proquest.com%2Fscholarly-journals%2Feffect-nursing-intervention-on-knowledge-practice%2Fdocview%2F2537156175%2Fse-2
- Seston, E. M., Magola, E., Bower, P., Chen, L., Jacobs, S., Lewis, P. J., Steinke, D., Willis, S. C., & Schafheutle, E. I. (2020). Supporting patients with long‐term conditions in the community: Evaluation of the Greater Manchester Community Pharmacy Care Plan Service. Health & Social Care in the Community, 28(5), 1671–1687. https://doi.org/10.1111/hsc.12992
- John, J. R., Tannous, W. K., & Jones, A. (2020). Outcomes of a 12-month patient-centred medical home model in improving patient activation and self-management behaviours among primary care patients presenting with chronic diseases in Sydney, Australia: A before-and-after study. BMC Family Practice, 21(1), 158–158. https://doi.org/10.1186/s12875-020-01230-w
- Heggdal, K., Mendelsohn, J. B., Stepanian, N., Oftedal, B. F., & Larsen, M. H. (2021). Health‐care professionals’ assessment of a person‐centred intervention to empower self‐management and health across chronic illness: Qualitative findings from a process evaluation study. Health Expectations : an International Journal of Public Participation in Health Care and Health Policy, 24(4), 1367–1377. https://doi.org/10.1111/hex.13271
- Fortmann, A. L., Gallo, L. C., Garcia, M. I., Taleb, M., Euyoque, J. A., Clark, T., Skidmore, J., Ruiz, M., Dharkar-Surber, S., Schultz, J., & Philis-Tsimikas, A. (2017). Dulce digital: An mHealth SMS based intervention improves glycemic control in hispanics with type 2 diabetes. Diabetes Care, 40(10), 1349–1355. https://doi.org/10.2337/dc17-0230
- Nguyen, N. T., Douglas, C., & Bonner, A. (2019). Effectiveness of self‐management programme in people with chronic kidney disease: A pragmatic randomized controlled trial. Journal of Advanced Nursing, 75(3), 652–664. https://doi.org/10.1111/jan.13924
- Dinh, H. T. T., Bonner, A., Ramsbotham, J., & Clark, R. (2019). Cluster randomized controlled trial testing the effectiveness of a self‐management intervention using the teach‐back method for people with heart failure. Nursing & Health Sciences, 21(4), 436–444. https://doi.org/10.1111/nhs.12616
- Wang, L., Mårtensson, J., Zhao, Y., & Nygårdh, A. (2018). Experiences of a health coaching self-management program in patients with COPD: A qualitative content analysis. International Journal of Chronic Obstructive Pulmonary Disease, 13, 1527–1536. https://doi.org/10.2147/COPD.S161410
- Kennedy, A., Rogers, A., Blickem, C., Daker-White, G., & Bowen, R. (2014). Developing cartoons for long-term condition self-management information. BMC Health Services Research, 14(1), 60–60. https://doi.org/10.1186/1472-6963-14-60
- Haslbeck, J., Zanoni, S., Hartung, U., Klein, M., Gabriel, E., Eicher, M., & Schulz, P. J. (2015). Introducing the chronic disease self-management program in Switzerland and other German-speaking countries: Findings of a cross-border adaptation using a multiple-methods approach. BMC Health Services Research, 15(1), 576–576. https://doi.org/10.1186/s12913-015-1251-z
- Arney, J. B., Odom, E., Brown, C., Jones, L., Kamdar, N., Kiefer, L., Hundt, N., Gordon, H. S., Naik, A. D., & Woodard, L. D. (2020). The value of peer support for self‐management of diabetes among veterans in the Empowering Patients In Chronic care intervention. Diabetic Medicine, 37(5), 805–813. https://doi.org/10.1111/dme.14220
- Yasmin, F., Yasmin, F., Banu, B., Banu, B., Sauerborn, R., Sauerborn, R., & Souares, A. (2020). The influence of mobile phone-based health reminders on patient adherence to medications and healthy lifestyle recommendations for effective management of diabetes type 2: A randomized control trial in Dhaka, Bangladesh. BMC Health Services Research, 20(1), 520–520. https://doi.org/10.1186/s12913-020-05387-z
- Benzo, R. P., Ridgeway, J., Hoult, J. P., Novotny, P., Thomas, B. E., Lam, N. M., V Benzo, M., Kramer, K., & Seifert, S. (2021). Feasibility of a Health Coaching and Home-Based Rehabilitation Intervention With Remote Monitoring for COPD. Respiratory Care, 66(6), 960–971. https://doi.org/10.4187/respcare.08580

Comments